Shoulder Impingement
Rotator Cuff Impingement
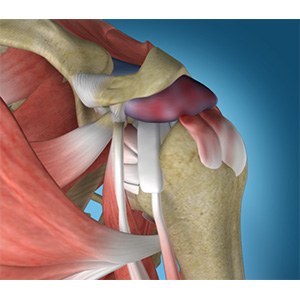
Impingement, bursitis, tendonitis, are all different words for the same underlying problem. The subacromial space is the space below the end of the shoulder blade (acromion) and top of the humeral head. Under normal circumstances, it is occupied by the rotator cuff which is a quarter of an inch thick and a bursa, which is a thin sac that covers the rotator cuff tendon and helps to lubricate and protect it from the abrasiveness from the bone during shoulder range of motion. The bursa is a normal structure with many nerve endings and can be found in any area in our body where a tendon or muscle is at risk of friction (knee, elbow, hip). Over time and with overuse, the bursal sac can become thickened and inflamed leading to pain. It is thought that certain individuals are more prone to developing this inflammation due to the anatomy they were born with and having a more down slope to their acromion. This is often termed a spur and creates less space available for the tendon to move. Much like a door that is too big and repetitively rubs on the carpet, over time this can lead to friction, inflammation, and ultimate fraying and tearing of the tendon as it repetitively rubs on the bone “spur” above. Conversely, persistent inflammation of the bursal sac may lead to irritation and blistering of the tendon and ultimately a tear. Whether the chicken or the egg comes first, this combination of bursitis (inflamed bursa) with tendonitis (inflamed tendon) is termed rotator cuff or impingement syndrome.
Symptoms
Patients with impingement syndrome can often times present very similar to that of a rotator cuff tear. The pain is usually localized laterally along the arm with radiation towards the mid/lateral humerus. It is generally worse with overhead activities such as reaching, driving or putting the dishes away and is intensified with weight. It may hurt at night but more when the affected shoulder is rolled upon. Occasionally, a feeling of a clicking sensation with shoulder motion may be noted as well. Strength is typically normal but patients will have a tendency to “give out” as a result of the pain they feel with resistance. Motion is also not routinely affected.
Differentiating impingement syndrome with a tear can often times be difficult but can be better deciphered based on history, age, duration and physical exam. An MRI or in-office ultrasound may be advised to make sure a tear is not the underlying cause of the pain. My rule of thumb is to image most patients with a history of traumatic onset, pain greater than 3-4 months, and weakness on examination specific to the rotator cuff musculature.
Treatment
The mainstay of treatment for impingement syndrome is conservative (non-operative) management. In fact, 80% of people with inflammation will improve simply with the combination of rest and time. Frequently, the condition will progress and create an ongoing chronic and frustrating problem. The natural tendency is to not use the arm when it hurts. This leads to weakness and atrophy of the rotator cuff muscles. The rotator cuff normally helps compress and dynamically stabilizes the shoulder joint. When it becomes weak, it is unable to resist the upward pull of the deltoid which is normally at equilibrium and the ball can pulled upward. This potentiates the impingement and makes things worse essentially creating a viscous cycle. Often times, to break this cycle, a subacromial steroid injection may be advised. The purpose of the medicine (steroid) is to shrink the bursa and halt the inflammatory process. This is equivalent to putting an ibruprofen tablet right where it needs to work, except this is a “super-tablet” that works higher up on the chain reaction to better halt the inflammatory cascade. Once the pain is improved, rotator cuff strengthening (Codman exercises) either at home or with a therapist is generally advised to re-strengthen the tendon and avoid the process from starting over.
In patients that fail to respond to conservative management, surgery may be advised. Patients that typically fall into this category are those that fail to gain any improvement following subacromial steroid injection. The surgery is performed arthroscopically with the intent to “burr the spur” and create more space for the tendon. Special attention is also paid to visualizing the rotator cuff and assuring that no high grade (greater than 50% width) partial thickness tearing of the tendon is present that may be require takedown and repair. Many clinical studies would support better outcomes in takedown and repair of partial high grade tears versus debridement alone in regards to pain relief and clinical outcomes.





